|
Neubauer Coporation
Getting your Trinity Audio player ready...
|
The gynecologist has compiled a complete guide on George V Magazine
The issue of contraception is relevant for any woman of reproductive age. Unfortunately, not everyone can (or wants) to understand the intricacies of this or that type of contraceptives. We spoke with obstetrician-gynecologist Dr. Nicole Zenner, who compiled a complete guide on modern contraception for George V Magazine.
Which contraceptive methods are the most questionable?
Unreliable methods include natural contraception:
- A calendar method of contraception based on the exclusion of sexual intercourse on the days of ovulation (the middle of the menstrual cycle, which corresponds to approximately 10–18 days from the start of menstruation). The contraceptive effect is low.
- Interrupted sexual intercourse. The contraceptive effect is low. Pearl index 4-18 per 100 women per year.
- Lactational amenorrhea method. Most women do not menstruate while breastfeeding. It is believed that if menstruation is absent, it is impossible to get pregnant. This is a harmful myth. The contraceptive effect is extremely low. The Pearl index, especially when the number of breastfeeding decreases, tends to 100.
The most reliable methods
Barrier contraception
Definitely a more reliable method than the natural one.
- Male condom. Pearl index 2-12 pregnancies per 100 women per year. High degree of protection against sexually transmitted infections.
- Female condom. Prevents sperm from entering a woman’s genital tract and reliably protects against infections. Pearl index 2-12.
- Vaginal diaphragm. Pearl index 6-18 pregnancies per 100 women. Does not protect against infections. Before starting your appointment, you must visit a gynecologist to select the correct size.
- Spermicides. Chemical preparations in the form of cream, gel, foam or vaginal suppository. The drug is administered vaginally, where it reduces sperm motility or destroys their membrane. The Pearl index is low: 3-21 pregnancies per 100 women. Often causes irritation of mucous membranes and does not protect against infections. When used simultaneously with a condom, it violates its integrity.
- Intrauterine devices are the so-called intrauterine devices. The spiral is inserted into the uterine cavity and does not allow the fertilized egg to implant into the uterine wall. Depending on the type of material, there are inert ones that release ions of gold, silver, and copper (these metals have an anti-inflammatory effect). There are more modern intrauterine contraceptives that release small amounts of hormones into the uterine cavity every day. In addition to the contraceptive effect, they have a pronounced therapeutic effect.High efficiency. Pearl index 0.5-1.0. Duration of action – 3 – 5 years or more.Among the disadvantages is a slight increase in the risks of ectopic pregnancy and inflammatory diseases of the pelvic organs when using non-hormonal IUDs.
Hormonal contraception
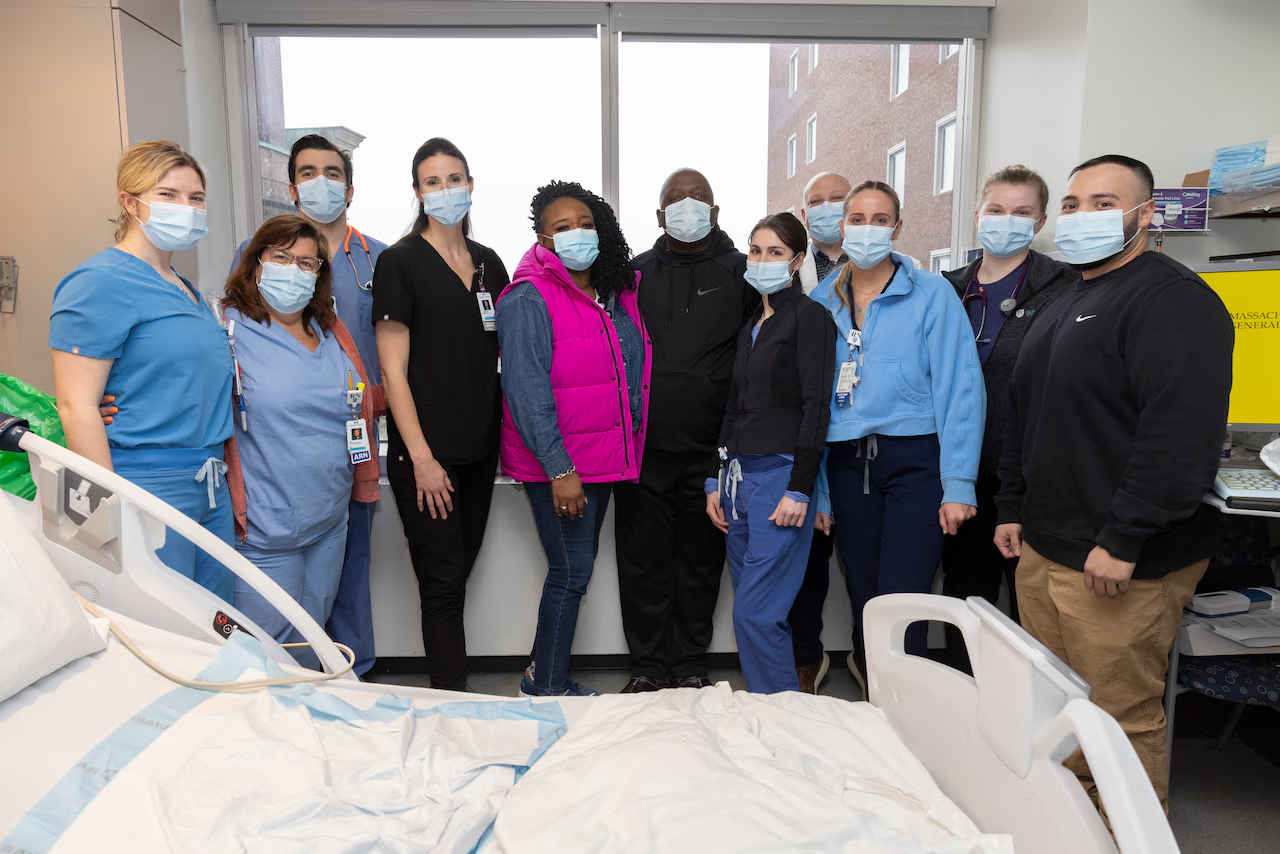
Dr. Nicole: “Hormonal contraception includes medications taken orally (pills), transdermally (patch), subcutaneously (implant) and vaginally (vaginal ring).”
Combined oral contraceptives contain female sex hormones estrogens and progestogens, which suppress ovulation and cyclic changes in the inner layer of the uterine cavity (endometrium), reduce sperm motility, and increase the viscosity of mucus in the cervical canal. When taking medications correctly, the Pearl index is 0.1. Oral contraceptives have a therapeutic effect for many gynecological diseases. Reduces pain in the first days of menstruation. They prevent the formation of ovarian cysts and prevent the occurrence of endometrial, ovarian and rectal cancer. Establish a regular menstrual cycle. They have a good cosmetic effect.
One of the disadvantages of the method is that when using tablets, you need to take the drug daily. Sometimes there is nausea at the beginning of use, increased appetite and decreased libido.
Any contraceptive medications cannot be combined with smoking. If there is a genetic predisposition to blood clots, they can cause a stroke or heart attack.
Based on estrogen content, hormonal contraceptives are divided into high-dose, low-dose, microdose and ultra-microdose. The lower the dosage, the safer.
Based on the combination of estrogen and progestogens, contraceptives are divided into monophasic and triphasic. The gynecologist warns that it is difficult to independently give preference to one or another type of hormones; consultation with a doctor is necessary. In this case, it is absolutely not necessary to take sex hormones. The doctor determines which type of drug is most suitable for a particular patient based on appearance and medical history (skin type, hair growth, weight, regularity of the cycle, presence of pregnancies, tendency to edema, etc.).
Dr. Nicole: “It is much more important before starting to take contraceptives to do an ultrasound of the mammary glands, take clinical and biochemical blood tests, and stop smoking, including electronic gadgets.”
Contraception (in any form) must be taken from the 1st to the 7th day of menstruation. Better in 1 – 3 days. After childbirth, contraceptives can be taken after 6 months if breastfeeding is stopped.
Convenient hormonal contraceptive methods include the subdermal implant, skin patch, and vaginal ring. There is no need to take daily pills.
There are hormonal contraceptives approved for use during breastfeeding. They contain only progestins. The drugs do not affect the quality and quantity of milk and the health of the child. Progestin-containing drugs are allowed for women who smoke.
Emergency contraception
The chemical composition of emergency contraceptive drugs is similar to hormonal contraceptives. Taken no later than 72 hours after unprotected sexual intercourse. The effectiveness of the method is high. Can be used no more than 2 times a year.